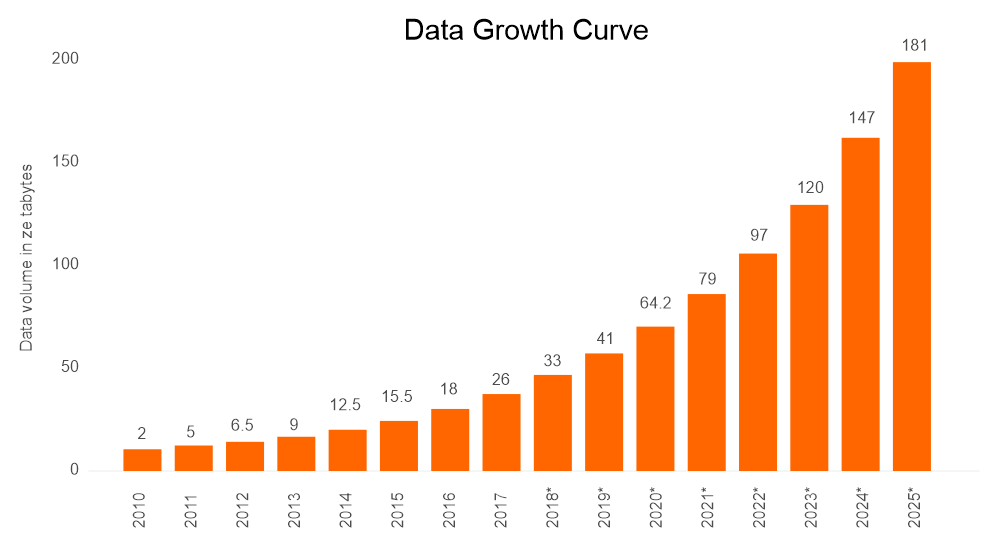
Data is in every facet of today’s modern society. Not only is there an exponential increase in the volume of data, but there is also more data in more places. The total amount of data created, captured, copied, and consumed globally is forecast to increase rapidly, reaching 64.2 zettabytes in 2020. Over the next five years, global data creation is projected to grow to more than 180 zettabytes.[1]
Organizations today are challenged to upgrade legacy tools and processes, and make sure data is housed properly in a secure and relevant way.
In healthcare, new technology standards are creating unique opportunities for patients and clinicians alike. Dr. William Stead from Vanderbilt University has estimated the number of data points, or facts, needed for a complex medical decision. In 1980, there were about 10 facts per decision. As of 2020, there were around 1,000 facts per complex decision. Making this more interesting, cognitive research, the study of the mind and its processes, shows that a human can handle only five to nine facts in a single decision.[2]
Prior to Covid-19, medical errors were the third leading cause of death in the U.S. after heart disease and cancer, according to a study by patient safety experts at Johns Hopkins University.[3] One can argue those critical errors were made because all the needed data was not readily available to make the most informed decisions. That is caused by the lack of a decision support system that could handle more than a handful of facts to help clinicians make the best choices.
The clinician’s ability to compute critical decisions on the fly, with limited facts, is due in part to large institutional clinical care systems, processes, and workflows being very much the same as they were decades ago. Doctors are already inundated with alerts and demands on their attention; tedious administrative tasks should be minimized so they can better focus on the patient in front of them, helping patients get high-quality care no matter where they seek it.
Even with newer technologies readily available, institutions still rely on pagers, faxes, email, and voicemail, which does not make for effective information sharing. One analysis, published in the Journal of Healthcare Management, suggests a 500-bed hospital loses over $4 million each year due to communication inefficiencies, with hospital physicians wasting around 45 minutes a day due to inefficient systems.[4] Technologies like FHIR, [pronounced "fire"] are a systemic game changer that facilitate lightning-fast exchange of pertinent clinical data and empower clinicians to make the best choices.
Fast Healthcare Interoperability Resources is the new standard developed by Health Level Seven International (HL7) as a platform for simultaneously accessing data from different healthcare systems, regardless of how the data is stored. Solutions built with the FHIR framework are modular.
The reusable components are called resources which can easily be assembled into working systems that solve real world clinical and administrative problems at a fraction of the price of existing alternatives.[5]
The Centers for Medicare & Medicaid Services (CMS) now requires regulated organizations to establish standards-based FHIR APIs, as specified by the ONC 21st Century Cures Act. This requirement presents challenges and opportunities as the healthcare system is typically a technology laggard. FHIR has the potential to change the way information is housed and consumed. It will allow data to be used in a wide variety of situations – mobile phone apps, cloud communications, EHR-based data sharing, server communication inside large institutional healthcare providers, and much more.
Opportunities to achieve greater efficiencies, lower costs, and attain higher degrees of effectiveness are great motivations to adopt FHIR. However, the most significant reason is that lives are literally at stake. For instance, an ER doctor knowing an important fact, like which medications the patient is allergic to, without having to comb through multiple sources and hope for the best. Having that patient-centered medical fact represented in a timely and relevant way is paramount to the best care and ultimately to the patient's life.
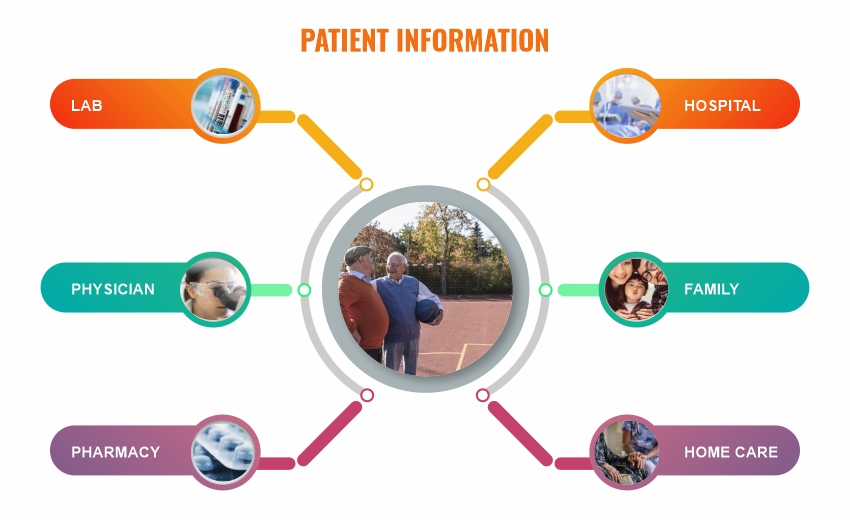
How does FHIR make all this possible? FHIR enables access to data distributed across systems, databases, and devices in real-time. Think of sites or apps that pull hotel, flight, or financial data to you whenever you need it. Using FHIR-based applications, clinicians in any situation can query for exactly the set of information required, such as medication history, allergies, or test results. FHIR helps providers avoid the burden of sifting through lengthy summary of care documents to get to the information they need at the time that they need it most.
FHIR conceptually is a representational state application programming interface, or a RESTful API. This means that instead of every fact being sent on a continuous feed or data stream as an all-in patient view, it can be queried simply, providing only the relevant information on-demand. FHIR offers many improvements over existing standards.[6]
How can your organization use this time of disruptive change to improve patient care and outcomes and compete more effectively in the market? Let Vee Healthtek help you move beyond the minimums of the government mandate!

Meeting the minimums of the CMS mandate. Creating a minimum viable product roadmap and gap analysis.
Raw components / data:
a. Disparate, non-standard, disconnected, inaccessible.
b. No implementation of FHIR standards.
c. Limited budgets for implementation.
d. No resources focused on interoperability.
e. Still sending and receiving "full" data feeds.
Standardized / curated data:
a. Data is secured, organized, and insightful.
b. Starting to use data more broadly internally for patient care.
Connected, accessible data and knowledge assets with data tailored for personalized care.
Test & Learn Cycle:
a. Establishing a data consumption plan, understanding your audience.
b. Building and implementing an API for the initial use cases to meet the mandate.
Let Vee Healthtek help you fully adopt FHIR for Internal and External data sharing to align your business and technology goals, improve and showcase patient outcomes across the care continuum, maximize clinician efficiency, and generate more revenue!
FHIR at its best, your company is now:
a. A data-driven organization.
b. Using Artificial Intelligence & Machine Learning.
c. Producing actionable insights as a core offering.
d. Using data for population your healthcare goals.
1: Amount of data created, consumed, and stored 2010-2025; Published by Arne Holst, Jun 7, 2021
2: Miller GA. The magical number seven plus or minus two: Some limits on our capacity for processing information. Psychological Review. 1956;63(2):81–97.
3: https://www.hopkinsmedicine.org/news/media/releases/study_suggests_medical_errors_now_third_leading_cause_of_death_in_the_us
4: https://pubmed.ncbi.nlm.nih.gov/20812527/
5&6: http://hl7.org/fhir/R4/summary.html