In this white paper, Jeff Shelmire, Senior Vice President Client Services, analyzes the key developments reshaping revenue cycle management and back-office processes. He discusses outsourcing revenue cycle management and medical coding operations as a strategy to combat these trends and allow health systems to focus on patient care.
Click on the video to the right to learn more about the author, his paper’s key takeaways, and his motivation for writing on this subject.
To discuss this white paper, please contact Jeff using the information provided at the bottom of the page.
The objective of this paper is to spotlight four developments that impact the face of revenue cycle management as we know it and, by extension, construct a different future for the back-office processes in healthcare.
Business leaders everywhere are evaluating what role large language models (LLMs) and associated generative artificial intelligence play in the enterprise. According to Wikipedia, “a large language model is a computational model notable for its ability to achieve general-purpose language generation and other natural language processing tasks such as classification.
Based on language models, LLMs acquire these abilities by learning statistical relationships from vast amounts of text during a computationally intensive self-supervised and semi-supervised training process.” This is one way machine learning happens. Over time, as the machine processes more and more data and makes the associated and appropriate correlation and inference from surrounding data, the efficacy of the artificial intelligence improves. That is, at least theoretically, the more data a machine processes, the “smarter” it becomes. This, of course, relies heavily on the accuracy of the data at the start of the entire process. It is a garbage-in-garbage-out type of scenario. Input > Processing > Storage > Output is the model by which computers run. AI and LLM do not change this core principle.

Health systems are starting to apply Generative AI and LLMs in revenue cycle management applications. Areas of early success have been centered around automating simple repeatable tasks that improve efficiency in coding and claims processing work. Presently, the use of AI and LLMs has been applied as a supplemental tool to automate administrative tasks to improve efficiency in coding and in claims processing. This, however, will change over time and these processes will become increasingly automated as the machines learn along the way.
Another area of early adoption has been in patient self-service. By applying LLMs and AI in call centers, health systems can provide easy-to-use and access to high-value information to patients. Patients can communicate with conversational AI, powered by LLMs, to schedule appointments, check billing information, get access to their medical records, and get answers to other common inquiries. This provides patients with 24/7 access to information, improves patient satisfaction, and lessens the administrative burden on the health system.
Data management is another area of adoption. LLMs take massive amounts of unstructured data, get it organized, and provide analytics and insights. This is especially helpful for applications such as HCC coding, where the page counts of medical charts routinely run into the 100s and copious amounts of information must be considered for accurate coding.
Predictive analytics built on these technologies can help health systems identify trends in the revenue cycle, such as payer behavior, claim denials, and payment delays. The results of the analysis can point to processes that need to be improved or revamped entirely.
Some of the top reasons a healthcare claim is denied by the payer are:

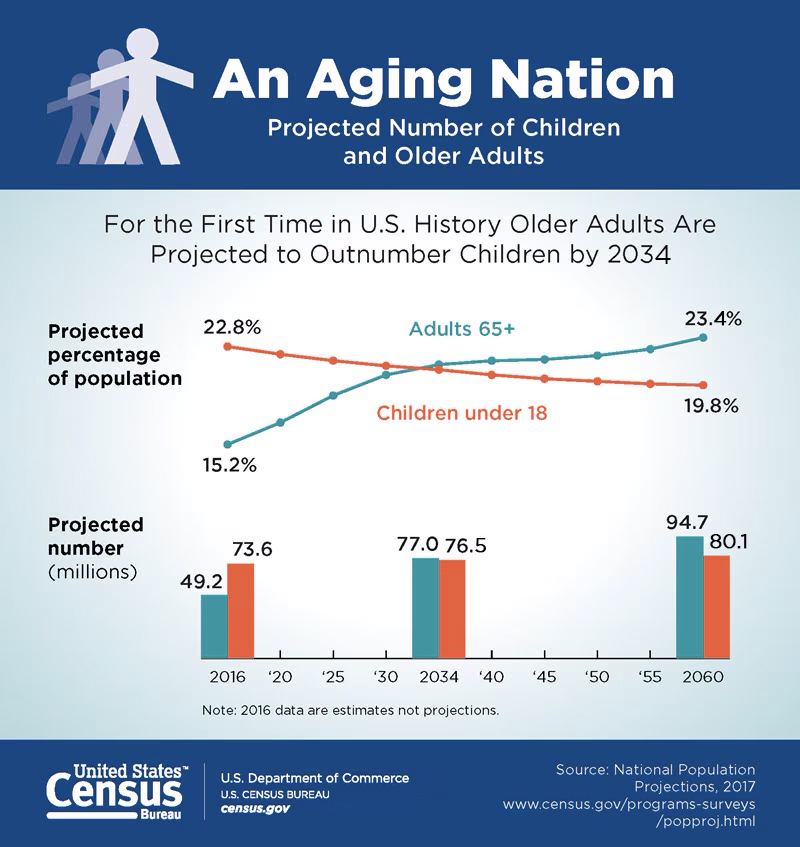
Healthcare costs continue to rise. The reasons for this are manifold. The aging American population is one contributor. As the population ages, more healthcare services are required to keep Americans healthy. Older people spend more on healthcare than their younger counterparts, and often, the procedures that older people get are more expensive — especially procedures such as joint replacements and heart surgeries.
In 2021, Americans older than 65 years of age comprised 16% of the population. By 2020, this percentage is expected to grow to 20%. Contributing to the rise in costs is also the rise in chronic illnesses. Chronic conditions, likewise, affect older people to a larger degree than younger people. According to the CDC, “in 2018, 51.8% (129 million) of civilian, noninstitutionalized adults had been diagnosed with at least one of ten selected chronic conditions. More specifically, 24.6% (61 million) of adults had one chronic condition, and 27.2% (68 million) had two or more chronic conditions.”
Health systems continue to confront rising labor costs and staffing shortages. The rising labor costs can be attributed to inflation, lack of supply, and high demand. For example, according to Zippia.com, the average age of a medical coder in the US is 45 years. There is a not a large crop of medical coders coming up behind the current professionals. With the advent of automation and artificial intelligence, medical coding is a discipline that will be largely automated within the next five to seven years.
Therefore, not many parents or career advisors are enthusiastic about the long-term prospects for individuals in this field. Granted, even when coding automation is widespread, human coders are still needed to audit and manually code edge cases that are too difficult to automate. According to a survey conducted by Health Management Academy, 47.5 percent of health systems currently use AI to help overcome labor shortages. The remaining 52.5 percent have plans to implement AI for the same reason. The application of AI in these settings is spread across back-office functions, clinical operations, and clinical care.
One strategy health systems have used in response to these trends is to partner with an outsourcing company.
Outsourcing RCM and medical coding operations to a partner has several benefits. Chief among them is that outsourcing firms have scale and specialized talent that health systems do not. Scale allows these suppliers to provide a comprehensive set of services with deep domain expertise in each. These providers frequently service many health systems and because of their scale, can staff substantial numbers of experts across the entire RCM and coding domains. Scale allows these firms the size and flexibility to process medical claims within service levels that many hospitals cannot manage.
Most companies turn work around within 24-48 hours with a minimum of 95% accuracy. This is especially helpful with fluctuations in patient volumes and the consequent change in RCM claims to be processed.
Moreover, since many of these firms have operations overseas in places like India and The Philippines, labor arbitrage becomes a vehicle for cost savings.
Outsourcing providers also incorporate automation and technology into their solutions. This eliminates the need for health systems to invest in the vetting, selection, and implementation costs associated with infrastructure, technology, and staffing.
With enhanced expertise and flexibility that scale brings, combined with cost savings and access to leading technologies, outsourcing is a viable mechanism for health systems to remain competitive. Furthermore, it frees health systems to spend resources and competencies on what they do best — deliver high-quality patient care.
www.mckinsey.com
www.outsourceaccelerator.com
www.economicsonline.co.uk
www.joinhorizons.com
www.revcycleintelligence.com
www.gebbs.com
www.ensemblehp.com
www.optum.com
www.outsourcestrategies.com
www.beckershospitalreview.com
https://en.wikipedia.org/wiki/Large_language_model
Generative AI’s Potential Shines on Revenue Cycle Management (revcycleintelligence.com)
www.zippia.com/medical-coder-jobs/demographics/
www.techtarget.com/healthtechanalytics/news/366590381/Almost-Half-of-Health-Systems-Use-AI-for-Workforce-Issues