Errors on prior authorizations were an ongoing problem for a healthcare system in the New Jersey area. Increased denials and other issues were leading to upset patients and a loss of revenue for the client. Additionally, the organization was facing internal staff turnover, and process directives were modified with each change in leadership. The superior performance and experience from our authorization management team provided an immediate turn around for our client.
Barriers to Overcome
A project was initiated for the client at the start of August 2018, with nearly 20% of the cases worked incurring an error. The authorization team was plagued with constant new directives, causing many challenges in the implementation of effective practices. The problems the team had to overcome included:
- Changes in client leadership with limited process training
- Minimal web portal access which led to additional phone time
- Increased volume of authorization requests lacking necessary information to process
- Internal challenges with changing directives
Solving the Problem
Led by the Manager at Vee Healthtek, and his team supervisor, the authorization team leaned on their previous years of experience and business rhythm to make an immediate impact. They led meetings twice weekly with the client and recorded best practice steps in a Standard of Practices (SOP) to limit and monitor the changes in processes. They also implemented a more sophisticated tracking system to record account progress, limit the number of errors and increase accuracy.
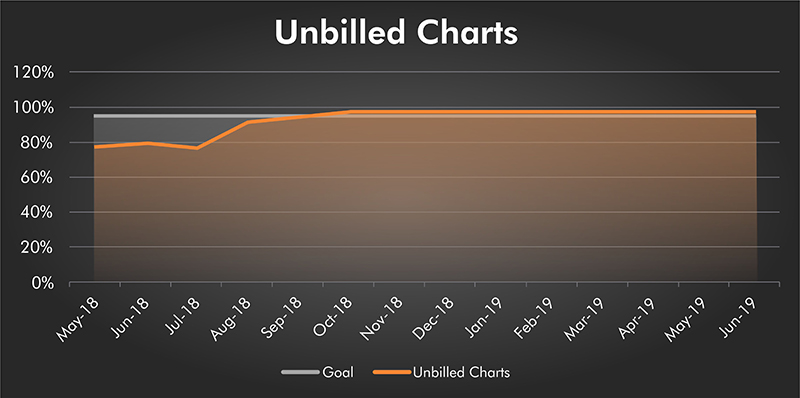
The chart below records the progress made by Vee Healthtek for the client:
Conclusion
The leadership and experience that our team brought was the differentiator between sub-par quality and exceeding client expectations. Within three months of initiating a plan and making process changes, accuracy increased from 80% to 98%. Accuracy remains ongoing at that level due to the great leadership of the Vee Healthtek team.
