In his white paper, Ed Scott, Client Services Director, introduces robotic process automation as a growing solution to hospitals and health systems’ greatest challenges. He discusses how Vee Healthtek used RPA to transform a client’s processes, which lowered employee turnover, reduced administrative burden, and decreased insurance claim denials.
Watch the video to the right to learn more about the author, his paper’s key takeaways, and his motivation for writing on this subject.
To discuss this white paper in detail, please reach out to Ed using the contact information provided at the bottom of the page.
Hospitals and health systems have been at the forefront of a major transformation while at a crossroads of increasing demand for higher acuity care and deepening financial instability. Persistent workforce shortages, severe fractures in the supply chain for drugs and supplies, and high levels of inflation have collectively fueled hospitals’ costs as they care for patients 24/7. At the same time, hospitals’ costs have been met with inadequate increases in reimbursement by government payers and increasing administrative burden due to inappropriate commercial health insurer practices.
Hospitals have seen significant growth in administrative costs due to improper practices by certain commercial health insurers. Commercial health insurers have overburdened hospitals with time-consuming and labor-intensive practices like automatic claims denials and onerous prior authorization and eligibility and benefits verification requirements.
A 2021 study by McKinsey estimated that hospitals spent $10 billion annually on dealing with insurer prior authorizations. Additionally, a 2023 study by Premier found that hospitals are spending just under $20 billion annually on appealing denials.
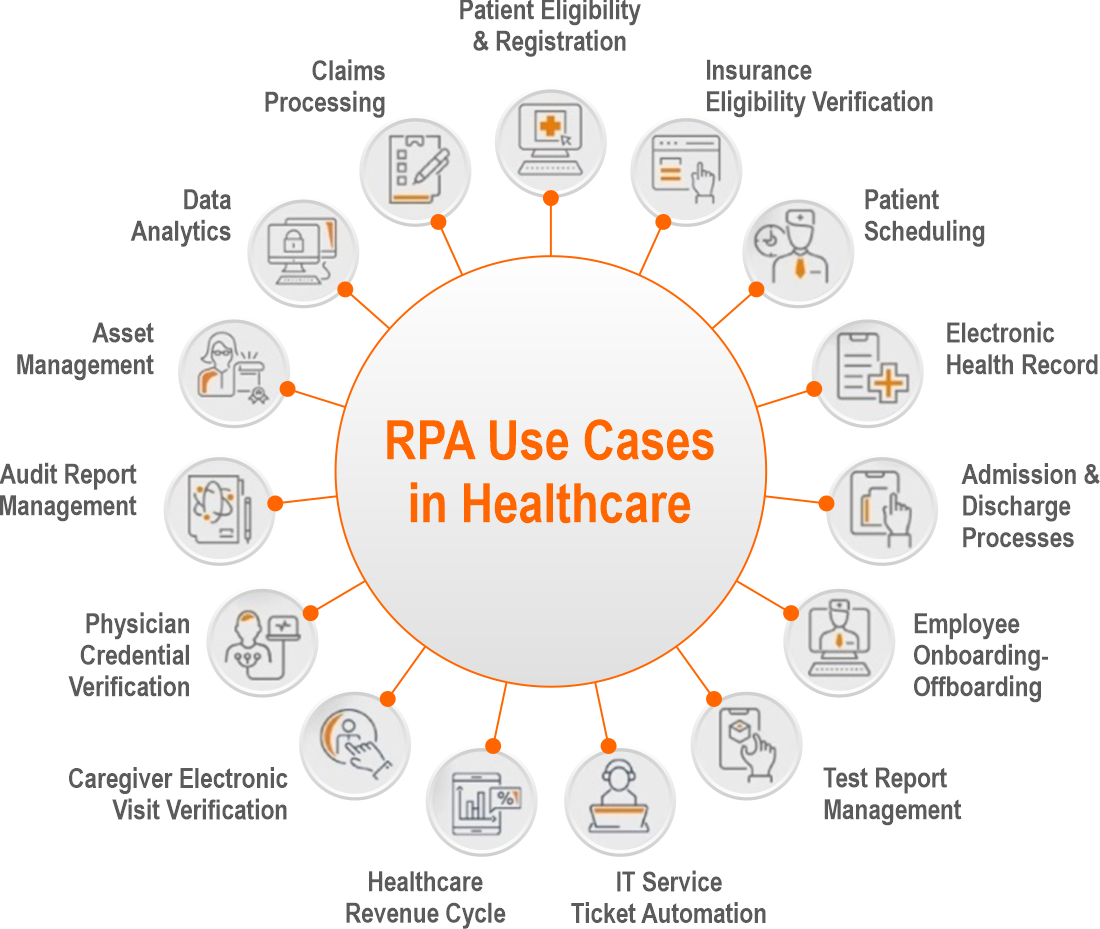
Robotic process automation is a fast-growing solution within the healthcare market today. Due to rising cost pressures, automation is a solution that will only continue to grow. The market size value in 2023 was estimated at $1.9 billion and to grow to $9.5 billion by 2030. This technology can eliminate repetitive rule-based tasks such as prior authorizations, eligibility, and benefit verification, as well as claims submission, to name a few. Additional benefits also include labor savings, reduction in errors that equate to fewer denials from the payers, and increased patient satisfaction with the reduction in delays to treatments due to the verification process.
Administrative errors can also be reduced and almost eliminated, allowing healthcare institutions to reallocate resources. This also coincides with increased savings from such repetitive tasks.
During one of my client’s Q4 governance meetings in 2022, the client stated that they wished to automate the factory. In early 2023, we added resources to manually assist with the eligibility and benefit verification process with the eventual goal of automating the process. At Vee Healthtek, we believe that understanding the manual processes and unique tasks required for each payer provides us with valuable insights into the optimal approach for implementing automation technology.
Moving into mid-2023, we were tasked to move forward with automating its top 10 payers. Initially, this was requested due to the daunting task of re-verifying coverages for all its patients at the beginning of each calendar year. This responsibility was given to its Patient Administrative Coordinators or PACS at each of its 150-plus locations. This task was daunting and was also one of the reasons it had an unusually high turnover ratio.
We put in place a business cadence meeting twice a week with the client and internal resources. Additionally, we collaborated with the client’s clearinghouse and its electronic medical record/practice management to build out bots where we were not able to build APIs (application programming interface) to grab pertinent information and properly populate its EMR.
Interestingly, some of the payer websites can detect automation and shut down the inquiry. Our team was able to mimic “human interaction” to bypass its detection system to complete the tasks.
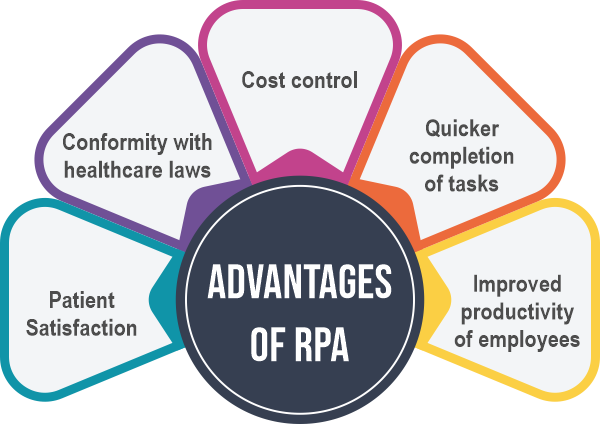
After automating the majority of the payers before the beginning of the year, the results were more than promising. The speed and efficiency resulting from the automation, which manually created a backlog of almost 6 weeks. By implementing the automation, the client re-verified the patients’ insurance information in a matter of a few weeks. In turn, its PACs have had a lower turnover rate, resulting in employee satisfaction, less administrative time, and lower costs. One of the most interesting metrics the client was able to calculate was a notable drop in insurance denials. Approximately 6% of its overall claims were denied by the payers for various reasons. With this solution, denials dropped to roughly 2%, which has resulted in additional cash flow, shortening the time for reimbursements. The next step with the client is to automate prior authorizations.
Here at Vee Healthtek, we work closely with our clients to understand their various needs rather than “selling” a service or solution. Our continuous communication is the key to success. As we conduct quarterly governance meetings with clients’ senior leadership, we discover gaps in workflow, inadequate technology, and various ways to increase cash flow. This is a prime example of how we work together with our clients to create outcomes that go beyond expectations.
The question now is… How can Vee Healthtek help you?
Robotic Process Automation in Healthcare Market projected (globenewswire.com)
https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-software-medical-device
https://www.aha.org/
https://www.mckinsey.com