In this white paper, Mark Kausel, Director Client Services, IT, discusses how Vee Healthtek assisted a Southeastern gastrointestinal practice management company with a $7 million credit balance issue following an acquisition.
Please click on the video to the right to learn more about the author, his paper’s key takeaways, and his motivation for writing on this subject.
To discuss this white paper in detail, reach out to Mark using the contact information provided at the bottom of the page.
Vee Healthtek works with a leading gastrointestinal (GI) practice management company in the Southeastern United States that focuses on building partnerships with physicians and practices across the country.
The company offers administrative services and operational infrastructure that includes finance, accounting, recruiting, information technology, human resources, marketing, and compliance. In 2019, the client acquired a specialty practice that had a $7 million credit balance dating back multiple years.
With the deadline of closing the books on the transaction looming and the risk of mis-valuing the acquisition and potential penalties from the government, the client engaged Vee Healthtek to research and categorize the balances for over 14,000 accounts in under 90 days. The client was extremely satisfied with the work and requested we look at other ways to support them.
As the credit balance project wound down, the client realized they were experiencing a dramatic loss in revenue due to an increase in volumes, and the internal staff unable to keep up creating a rapidly growing backlog. Because prior authorizations were not able to be obtained in a timely manner, appointments were being canceled or rescheduled at the last minute creating unused appointments and lost revenue.
The variation in processes for each payer created a growing backlog that adversely affected patient care, and the financial performance of the client’s endoscopy centers and practices. It created an increase in having to cancel patient appointments, sometimes after they arrived for the procedure, and an increase in denials if services were rendered without prior authorization being obtained. It also meant that patients were often uninformed about their out-of-pocket responsibilities prior to arriving for an appointment. This situation created lost revenue opportunities, increased frustration from the office staff, and very unhappy patients resulting in lower patient satisfaction scores. More importantly, patients were not getting the care they needed.
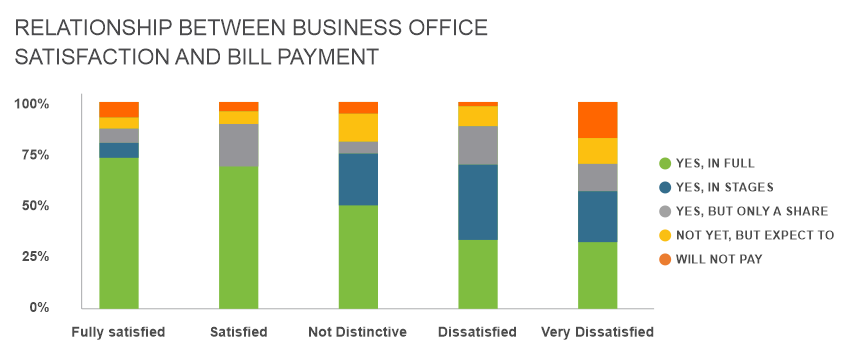
Surprising patients with unexpected healthcare costs may not only affect the consumer’s business office interaction, but also the healthcare organization’s operating costs. Sixty-three percent of consumers with payments that exceeded their expectations have or will call the healthcare organization’s business office, increasing the number of calls and the staff required to support those volumes. In comparison, 70 percent of consumers with healthcare balances that met expectations will not call the business office. i
The client turned to Vee Healthtek to provide reliable, scalable, and high-quality prior authorization services to quickly reduce their growing backlog and provide an ongoing solution. A dedicated offshore delivery team was deployed within one week to support the client. The Senior Manager of Operations and Client Operations Director spent a significant amount of time on-site learning and refining the client’s processes, training the Vee Healthtek team in India, and building strong relationships with the client’s management team.
Vee Healthtek deployed Sona ProMISe as part of our solution. This workflow management tool ingests the appointment details multiple times each day and allows work to be assigned based on predictive analytics enabled by the client’s business rules. This state-of-the-art tool provides real-time reporting through dashboards, enabling supervisors to monitor workloads and rebalance as necessary to ensure service level agreements are met and expectations are exceeded. Finally, ProMISe supports our industry-leading quality assurance program by randomly selecting appointments to assign to the QA process. The real-time reporting feature enables supervisors to monitor productivity and quality for each employee.
The client performs over 450 outpatient procedures daily, along with office visits, infusions, and ancillary visits with growing volumes. At the outset, there were over 5,000 appointments in the backlog that needed to be worked. For each appointment, Vee Healthtek needed to perform the insurance verification and eligibility check and determine if a prior authorization was required. If it was, Vee Healthtek initiated the request for the prior authorization. The client has more than twenty payers, each who had their own process for obtaining a prior authorization.
Some payers allow requests to be made through their portal, while others required multiple telephone calls, and in some cases, forms needed to be completed and submitted. All this work needed to be documented in the practice management system and available to support office staff with documentation of each patient’s financial responsibility and claims submissions to effectively manage denied claims. By implementing best-practices, and deploying this technology, our team was able to streamline and prioritize the inventory of appointments based on payers who require authorizations and individual payer turnaround times to obtain authorizations.
Accurate and timely information was communicated to the client’s Financial Counselors who contacted patients prior to their appointments to provide estimates of each patient’s financial responsibility. Implementing recommendations to schedule patients based on each payer’s turnaround time also improved outcomes, saved money, and increased patient and staff satisfaction.
The solution Vee Healthtek delivered has provided substantial results for our client. The denial rate due to authorizations decreased from 15% to 2%. We also reduced the rate of cancelations from the prior authorization backlog from 12% to 0%. All appointments are now worked within three days of the appointment creation date and fourteen days prior to the appointment date. The client is no longer experiencing the significant revenue leakage for failing to obtain authorizations in a timely manner and is on track to deliver one of their best years.
We exceeded the client’s expectations through rapid skilling and education, deploying a full-scale team, and providing partnerships to deeply understand the challenges they were facing. Extraordinary Outcomes: from patient complaints to patient praise, from no-shows to fully booked appointment schedules, from surprise patient bills to value-based care and transparency. Vee Healthtek delivered.
ihttps://revcycleintelligence.com/news/healthcare-business-office-experience-impacts-patient-collections