In care delivery, 94% of physicians say prior authorizations (PAs) result in delays. Patients go untreated for longer because of an opaque, complicated approval process. Or they just abandon care as being too hard.1
Not intending to create barriers, 98% of health plans use peer-reviewed, evidence-based studies when designing their prior authorization programs. They expect to improve quality and promote well-grounded criteria. 2
Strife Evidence
But 74% of physicians score payers’ PA criteria as only sometimes, rarely, or never evidence-based.1 A recent 14M-claim study justified their assessment. 25% of Medicare Advantage services, by net reimbursement, required a PA but would not if billed under CMS guidelines.3 Most payers extend these Medicare Advantage rules to their commercial plans, so we have an endemic problem.
Payer rules, in addition to clinical evidence, must then steer physician decisions. Hidden payer logic undermines physician expertise and costs them valuable time. 85% of physicians count their 40 prior authorizations per week as a high or extremely high burden.1 Frustrated by insufficient time to document their decision details, this increases physician burnout prevalence by 5.8X.4
For physicians, the criteria used for PAs are unclear. They rarely know at the point-of-care if the prescribed treatment requires prior authorization. They only find out later when a patient’s access is delayed or denied.5
PAs form a bitter barrier to patient care that:
- Delay or scrap patient treatment,
- Cost physicians valuable time,
- Reduce reimbursement for already-provided services, and
- Undermine their expertise.5
Process Transformation
A group of leading providers and payers with remarkably diverging interests have expressed consensus for dramatic PA change, including “communication and collaboration.”6 But prospects for transformation are poor.
At Vee Healthtek, we transform the PA process one patient, one physician, and one healthcare system at a time. Our framework assesses historical data, processes, system interfaces, training and automation using RevAmp, our automation workflow platform, to completely transform the PA process.
With an integrated Prior Authorization Program we work backward from denied claims, which for one new client reached 22% of revenue. Using RevAmp analytics, we sift through claims history to assemble clusters of denied accounts into a Pareto diagram of chronic root causes. With workflow maps, decision dependencies, and training scenarios we assemble intelligence on critical gaps into an efficient program for high approval rates.
Invariably, our solution starts at the front of the revenue cycle. We drive quality forward in the process. For a patient’s diagnosis requiring a procedure or medication, plan eligibility research may trigger a PA.
That’s when the hard work starts. Success rests on researching and gaining a thorough understanding of the current rules from the payer plan for this member. Without clear criteria, a PA request is destined for denial.
- 86% of initial denials have incomplete support from clinical information
- For 93% of final denials, the procedure or medication is not clinically appropriate based on payer assessment of the medical literature or clinical guidelines2
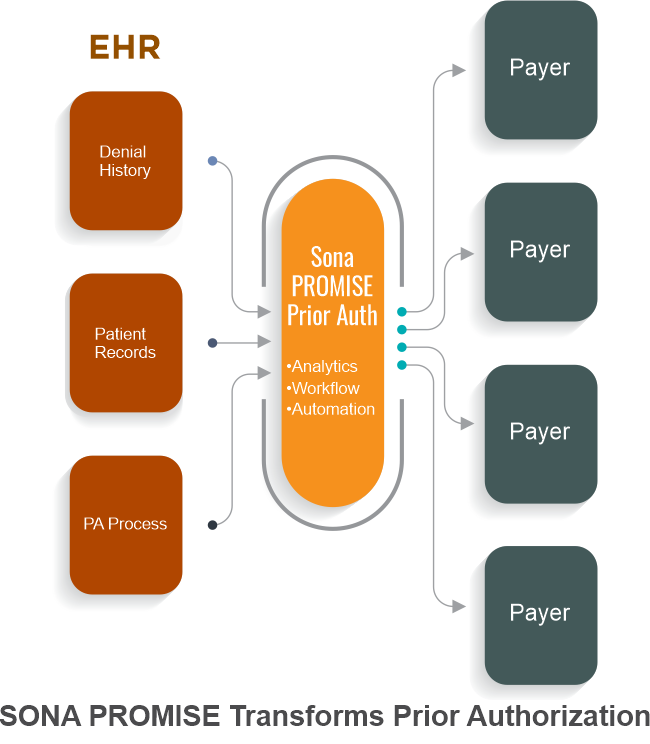
When a physician orders a procedure, test, or medication, we traverse payer-imposed process steps. Centralizing the entire process using RevAmp, we inventory clinical requirements and payer rules to map the scenario for approval.
On the payer’s website or the phone, we assess the member’s plan for relevant criteria and overlay the physician’s orders onto those rules. Working from the medical record, we match documentation with payer requirements. With a clean match, we fill the forms from patient EHR records and submit the compliant request.
When documentation is insufficient, we record the criteria and gaps for physician staff in the EHR. With a clear line of sight, the physician can determine whether and how documentation of their findings can comply with the requirements. With light physician involvement, we submit a compliant package.
Hound the Payer
Through the EHR, website, phone, email, fax, and API we monitor the payer for approval or rejection. We follow up in real time when care is in the balance. If denied, we assess the gap and go back to the physician’s staff for data to resubmit. If the gap can’t be filled but the physician disputes the criteria, we facilitate a peer review. Vee Healthtek drives for the highest PA success rate with the least provider impact. Our goal is to gain authorization up front for all requests. But it’s not unusual for denials to arise at claim submission. We work both the easy cases and the hard ones.
- Detailed denial inspection can permit a correct resubmission.
- Coding from the encounter can cause a rejection because the medical record doesn’t match the terms of the authorization. An error in coding or HIM records can be resubmitted correctly.
- For a procedure mistakenly performed without a required PA and rejected, we gather the required documentation to immediately submit a retro-authorization.
- In a surprising number of cases, glitches in the payer’s system logic cause them to not follow their own authorization rules. With solid documentation from eligibility confirmation onward, we inevitably resolve these for the patient.
If all this sounds breathtakingly tedious, and it is. Not to worry. With historical experience of provider documentation gaps and payer behavior, we apply RevAmp's automation functionalities to the high-volume, repetitive parts. Automation drives down the healthcare system’s cost to collect and further eliminates errors from manual transactions while delivering the transformed PA success rate.
Transformation Results
With RevAmp and the discipline of our prior authorization program, our clients reverse the trend, delivering effective care with:
- Faster care for more patients,
- Lower clinical administration burden,
- Higher proper reimbursement for medically necessary procedures
- The highest use of physicians’ judgment
Vee Healthtek enables physicians to focus on delivering patient care without barriers.
References:
1. 2020 AMA Prior Authorization PA Physician Survey. American Medical Association. https://www.ama-assn.org/system/files/2021-04/prior-authorization-survey.pdf
2. AHIP. 2019. Key Results of Industry Survey on Prior Authorization. https://www.ahip.org/wp-content/uploads/Prior-Authorization-Survey-Results.pdf
3. Schwartz, et al. 2021. Measuring the Scope of Prior Authorization Policies – Applying Private Insurer Rules to Medicare Part B, JAMA Health Forum. 2021;2(5):e210859. doi:10.1001
4. Olson, et al. 2018. Cross-sectional survey of workplace stressors associated with physician burnout measured by the Mini-Z and the Maslach Burnout Inventory. Stress Health. doi: 10.1002/smi.2849
5. Prior authorization hurts patients, physicians, and employers. It’s time to #FixPriorAuth. 2021. FixPriorAuth.org. https://fixpriorauth.org/
6. Consensus Statement on Improving the Prior Authorization Process. 2021. AMA, AHA, APhA, AHIP, BCBS, and MGMA. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/arc-public/prior-authorization-consensus-statement.pdf
